Recognizing Arrythmia’s with Nurse Brennan
The early recognition and intervention of cardiac arrythmia’s can be critical in promoting adequate perfusion and circulation, and in preventing irreversible outcomes or patient mortality. Not every arrhythmia is dangerous, and it is imperative to know your patient’s baseline heart rate and rhythm to triage any concerns as they arise. Whenever possible, a 12-lead EKG should be obtained when a patient experiences a new cardiac arrhythmia. With any cardiac arrhythmia, it is important to identify and treat the underlying cause (e.g. hypoxia). In the event of cardiopulmonary failure, following the ABCs and initiating CPR is necessary, with intubation, the administration of oxygen, and establishing IV/IO access as important interventions. A Zoll or defibrillator should also be present in case the patient requires defibrillation or synchronized cardioversion.
Below are 10 cardiac rhythms that you may encounter as a Medliant USRN. Do not be overwhelmed with the different types of cardiac rhythms and how to treat them. The most important takeaway as an RN is to be able to recognize when a cardiac rhythm is abnormal and to inform the practitioner or physician immediately. Caring for our patients is a team effort and the early recognition of an abnormal presentation is always the most critical step in being able to treat it.
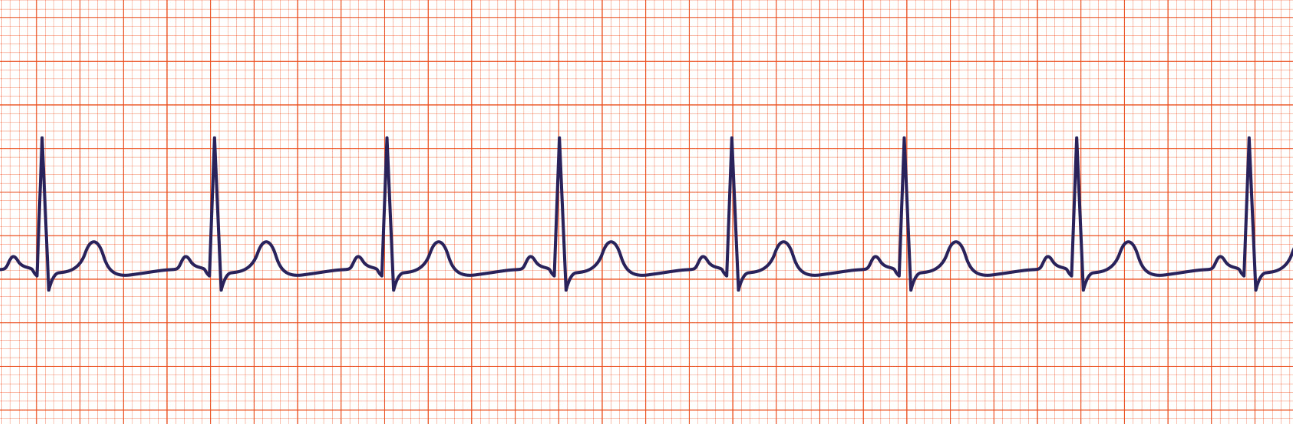
1. Normal Sinus Rhythm: Characterized by a normal P-wave, QRS complex, and T-wave. The normal heart rate is between 60-100 bpm while at rest for a healthy adult patient.
2. Sinus Bradycardia: A regular sinus rhythm with a visible P-wave and a heart rate of less than 60bpm. Hypoxia is a leading cause of symptomatic bradycardia, and a full set of vital signs should be taken to assess the SPO2 and blood pressure. Other causes may include cardiomyopathy, myocarditis, acidosis, hypotension, hypothermia, drug effects, and increased vagal tone as a result of suctioning, gagging, or vomiting. Sinus bradycardia may not always be a concern, such as with patients who are asleep or conditioned athletes who have a high stroke volume and increased vagal tone. For persistent bradycardia, epinephrine will often be the first drug of choice, followed by atropine.
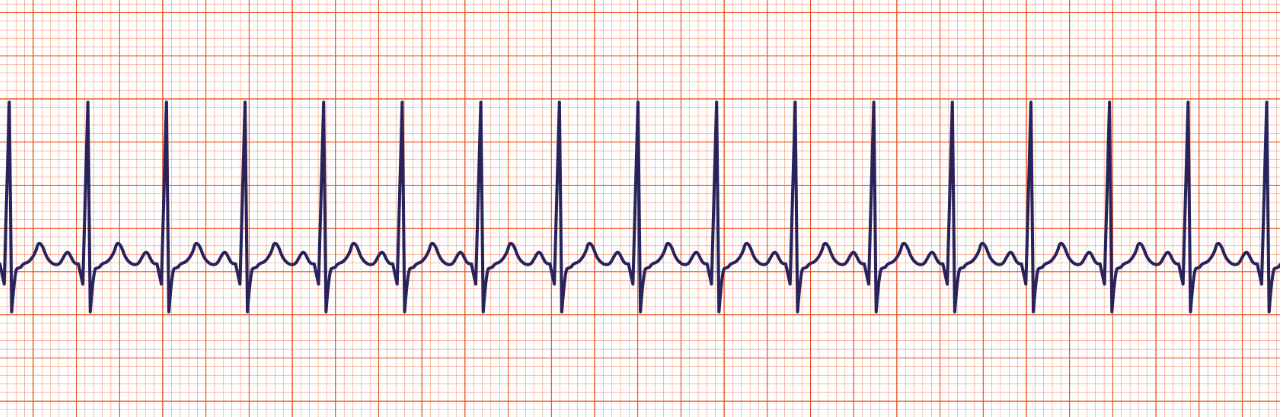
3. Sinus Tachycardia: A regular sinus rhythm with a visible P-wave and a heart rate greater than 100 bpm. This may be caused by exercise, pain, anxiety, hypoxia, hypovolemia, fever, shock, toxins or poisons, anemia, cardiac tamponade, tension pneumothorax, or a thromboembolism. Sinus tachycardia is often a response to an increased oxygen demand.
4. Supraventricular Tachycardia (SVT): A fast heart rate with narrow and regular QRS complexes. P-waves are difficult to observe with SVT. This is the most common type of tachycardia. SVT is not always detected and may even persist for hours or days if symptoms are not recognized. If unresolved, SVT can lead to impaired myocardial function, hypotension, altered mental status, weak peripheral pulses, lethargy, and cool extremities. A vagal response will often be stimulated in an attempt to escape SVT. If unsuccessful, adenosine may be initiated if the patient is stable. If the patient becomes unstable, synchronized cardioversion is often necessary.
5. Atrial Flutter (AF or A Flutter): A fast atrial heart rate with a “sawtooth” pattern of P-waves. Conduction from the P-waves to the QRS is variable, hence a QRS complex does not always succeed a P-wave.
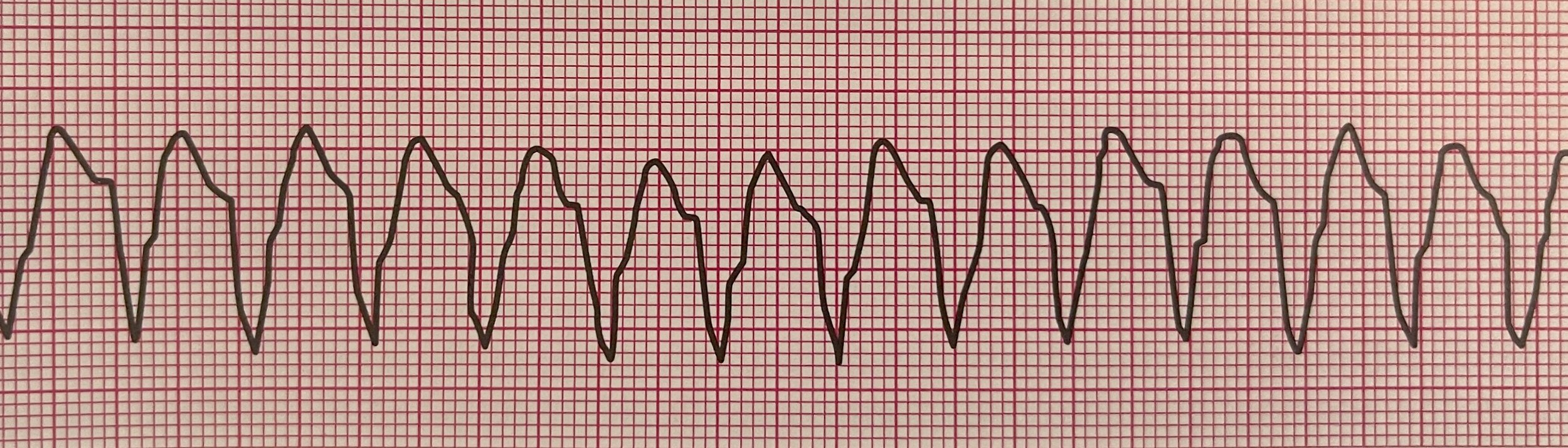
6. Monomorphic Ventricular Tachycardia (VT): An abnormally fast, regular, and widened set of QRS complexes with no visible P-waves. The QRS complexes are all identical or monomorphic in nature. This rhythm can precede ventricular fibrillation and may be fatal if not treated. Patients with VT often have a family history of cardiac disease. VT can also result from electrolyte imbalances such as hyperkalemia, hypocalcemia, or hypomagnesemia, as well as drug toxicity or coronary artery abnormalities.
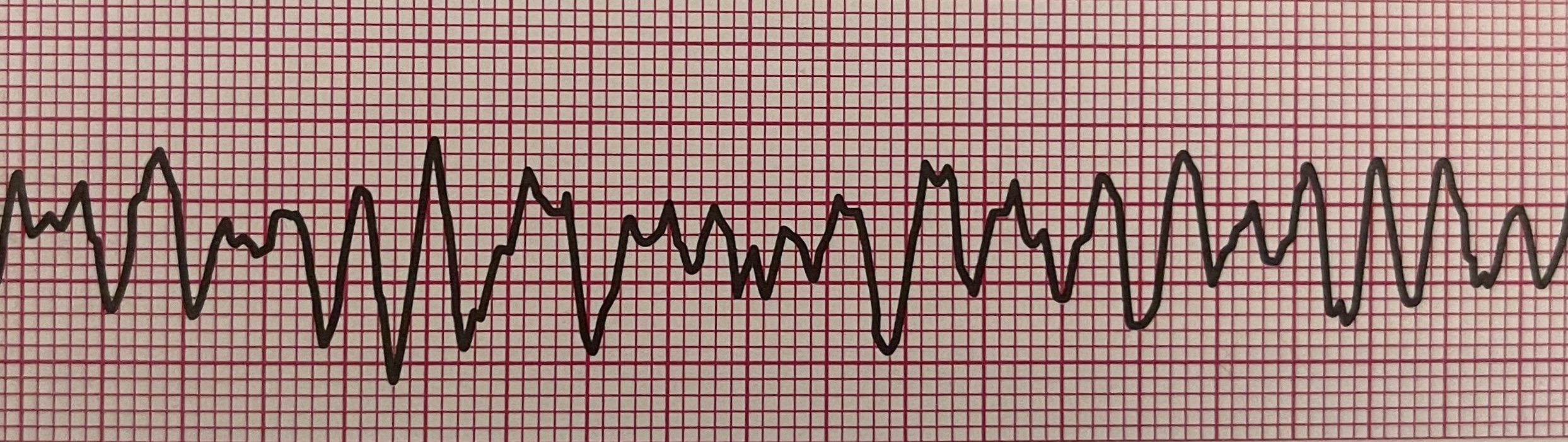
7. Polymorphic Ventricular Tachycardia: Similar to monomorphic ventricular tachycardia, QRS complexes are widened, however, with polymorphic ventricular tachycardia, QRS complexes will be irregular and are not identical in their appearance.
8. Torsades de Pointes: This is a specific type of polymorphic ventricular tachycardia. Torsades de Pointes is often referred to as the “turning of points” and presents with a QT interval that is prolonged at the base. QRS complexes will often appear as if they rotate around the ECG isoelectric line. It can be caused by long QT syndrome, hypomagnesemia, hypokalemia, or drug toxicity.
9. Ventricular Fibrillation (VF or VFib): There is no definable QRS complex with ventricular fibrillation. It will often present as an irregular and chaotic or disorganized heart rhythm. Defibrillation is necessary.
10. Pulseless Electrical Activity (PEA): This can be any organized heart rhythm, however, the patient will be unresponsive with no palpable pulses.
Sources:
ACLS Medical Training (2022). Rhythm Recognition. Retrieved from: https://www.aclsmedicaltraining.com/rhythm-recognition/
American Heart Association (2020). Pediatric Advanced Life Support Provider Manual.
American Heart Association (2020). Advanced Cardiac Life Support Provider Manual.